Understanding Perimenopause and Its Impact on Menstrual Cycles
Perimenopause, often referred to as the menopausal transition, is a significant phase in a woman’s life that typically begins in the late 30s to early 50s. It represents the period leading up to menopause, during which the ovaries gradually produce less estrogen. As hormonal fluctuations become more pronounced, menstrual cycles become irregular, often causing confusion and concern. Many women experience changes such as spotting during perimenopause, periods getting closer together in their 40s, or brown discharge, all of which can raise questions about what is normal and when to seek medical attention.
You may also like: How Long Does Perimenopause Last? Understanding the Timeline, Symptoms, and What to Expect
The unpredictable nature of perimenopausal bleeding stems from shifting levels of estrogen and progesterone, two hormones that regulate the menstrual cycle. As these levels fluctuate, the uterine lining may build up inconsistently, leading to unpredictable bleeding patterns. This can result in perimenopause spotting instead of a period, prolonged bleeding, or even instances where a woman experiences a perimenopause period every two weeks. Understanding these variations and distinguishing between normal perimenopausal symptoms and those that require medical intervention is crucial for navigating this transition with confidence.
What Does Your Period Look Like During Perimenopause?
One of the most common concerns among women undergoing perimenopause is the unpredictable nature of their periods. Many wonder, “What does your period look like during perimenopause?” The answer varies significantly from woman to woman, but some general patterns emerge. Periods may become heavier or lighter, longer or shorter, and may occur at irregular intervals. Some women experience perimenopause spotting all month, while others notice their menstrual cycle getting shorter in their 40s, leading to more frequent periods.
Perimenopausal bleeding can present in different forms. Some women experience light spotting between periods, while others have periods that are much heavier than usual. Additionally, brown discharge during perimenopause is a common occurrence, often indicating old blood leaving the body. Such variations are primarily due to hormonal imbalances that affect ovulation and the shedding of the uterine lining. While these changes can be unsettling, understanding that they are part of the normal aging process can help alleviate anxiety.
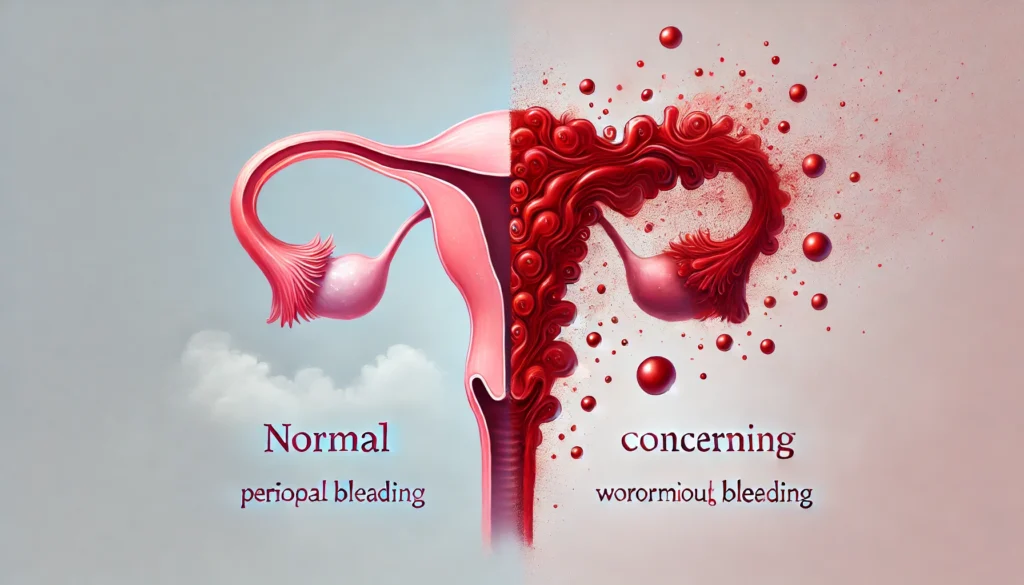
When to Worry About Perimenopausal Bleeding
Despite the wide range of normal menstrual changes during perimenopause, certain symptoms may indicate underlying health concerns that require medical attention. The question “When to worry about perimenopausal bleeding?” arises when bleeding patterns become excessively prolonged, heavy, or accompanied by other alarming symptoms.
One red flag is experiencing perimenopause bleeding for three weeks or longer. While some irregular bleeding is expected, excessively long periods may signal hormonal imbalances that need to be addressed. Similarly, if a woman experiences perimenopausal bleeding between periods frequently, it may indicate issues such as endometrial hyperplasia, fibroids, or even early signs of uterine cancer.
Other concerning symptoms include passing large blood clots, experiencing severe pelvic pain, or having a perimenopause period every two weeks persistently. If these symptoms arise, seeking medical evaluation is crucial. A healthcare provider may recommend blood tests, ultrasounds, or even a biopsy to rule out serious conditions and provide appropriate treatment.
The Causes of Perimenopause Spotting and Irregular Bleeding
Perimenopausal spotting and irregular bleeding can be attributed to several factors, most of which are linked to hormonal fluctuations. As estrogen levels decline, the uterine lining may become unstable, leading to spotting between periods. Additionally, perimenopause spotting instead of a period can occur when ovulation becomes irregular, preventing the normal shedding of the uterine lining.
Another contributing factor is progesterone deficiency. Progesterone helps regulate the menstrual cycle by stabilizing the uterine lining. When progesterone levels drop, the lining may break down unpredictably, causing intermittent bleeding. This explains why some women experience perimenopause spotting all month or prolonged spotting that seems never-ending.
Fibroids, polyps, and endometrial hyperplasia are other potential causes of irregular bleeding. These conditions often become more prevalent during perimenopause and can contribute to symptoms such as spotting during perimenopause or unusually heavy bleeding. Consulting a healthcare provider can help determine whether medical intervention is necessary to manage these conditions effectively.
Managing Perimenopausal Bleeding and Maintaining Hormonal Balance
For many women, perimenopausal bleeding can be managed through lifestyle adjustments, hormone therapy, and medical treatments. Understanding how to regulate hormone levels can significantly improve quality of life during this transition.
Hormone replacement therapy (HRT) is a common approach for managing severe symptoms, including frequent and heavy bleeding. HRT can help stabilize estrogen and progesterone levels, reducing the unpredictability of menstrual cycles. However, HRT is not suitable for everyone, and risks must be weighed against benefits.
Lifestyle changes also play a crucial role in managing perimenopausal bleeding. Regular exercise, a balanced diet rich in phytoestrogens (such as soy products and flaxseeds), and stress management techniques like yoga and meditation can help regulate hormones naturally. Additionally, certain supplements, such as vitamin D, magnesium, and omega-3 fatty acids, may support hormonal balance and improve menstrual symptoms.
For women experiencing severe perimenopausal bleeding for two months or longer, medical interventions such as endometrial ablation or intrauterine devices (IUDs) may be recommended. These treatments can help reduce excessive bleeding and provide long-term relief.
Frequently Asked Questions (FAQ) on Perimenopausal Bleeding
1. What does your period look like during perimenopause?
Perimenopause can cause significant changes in the appearance and consistency of menstrual flow. Some women experience heavy, prolonged bleeding, while others notice a lighter, shorter flow. It is common for periods to become erratic, sometimes starting and stopping unpredictably or appearing as perimenopause spotting instead of a period. Brown discharge during perimenopause is also frequent, often signaling older blood leaving the uterus at a slower rate. The texture of menstrual flow can vary from watery to thick, with occasional clots, depending on hormonal shifts and how the uterine lining is shedding.
2. When should I worry about perimenopausal bleeding?
While irregular bleeding is a hallmark of perimenopause, certain patterns warrant medical evaluation. If perimenopause bleeding lasts for three weeks or longer, it could indicate underlying conditions such as fibroids, endometrial hyperplasia, or hormone imbalances. Sudden, excessively heavy bleeding that soaks through pads or tampons within an hour should also be a cause for concern. Additionally, perimenopausal bleeding between periods or postmenopausal spotting should be assessed to rule out endometrial cancer or other serious conditions. It is crucial to track your symptoms and discuss any concerning changes with a healthcare provider.
3. Why are my periods getting closer together in my 40s?
Many women notice that their periods are getting closer together in their 40s due to shortened cycles caused by fluctuating estrogen and progesterone levels. As ovulation becomes inconsistent, the body may release eggs more frequently or skip ovulation altogether, leading to perimenopause periods closer together. A perimenopause period every two weeks is not uncommon and can result from a rapidly thickening uterine lining that sheds more often. Although this change is typically hormonal, conditions like polyps or thyroid disorders can also cause frequent bleeding, so persistent changes should be evaluated.
4. Is spotting normal during perimenopause?
Spotting during perimenopause is common due to fluctuating hormone levels affecting the stability of the uterine lining. Some women experience perimenopause spotting all month, especially if estrogen dominance causes the lining to shed irregularly. Perimenopausal bleeding between periods can also occur due to increased vascular fragility in the uterus. While occasional spotting is generally not a cause for concern, persistent or postmenopausal spotting should be discussed with a healthcare professional to rule out any underlying issues.
5. Can perimenopause cause bleeding for two months straight?
Perimenopausal bleeding for two months is not typical and may indicate an underlying medical condition. Continuous bleeding can result from endometrial hyperplasia, fibroids, or hormone therapy side effects. A persistently thickened uterine lining that does not shed properly can also lead to prolonged bleeding. If you experience perimenopause bleeding for three weeks or longer, or if the bleeding is excessively heavy, it is essential to seek medical advice. Treatment options such as hormone therapy, endometrial ablation, or medication may be recommended to regulate the cycle and prevent excessive blood loss.
6. Why is my menstrual cycle getting shorter in my 40s?
A shorter menstrual cycle during perimenopause is primarily due to declining ovarian function. As the ovaries produce less estrogen, the follicular phase—the time leading up to ovulation—shortens. This results in periods getting closer together in the 40s, often leading to a perimenopause period every two weeks. Shortened cycles can also be exacerbated by stress, lifestyle changes, or medical conditions such as thyroid dysfunction. While shorter cycles are usually part of the normal transition to menopause, sudden, extreme changes should be discussed with a doctor.
7. What causes brown discharge during perimenopause?
Brown discharge during perimenopause is usually old blood that has taken longer to exit the uterus. It often occurs at the beginning or end of a period when the flow is lighter. Hormonal fluctuations can cause irregular shedding of the uterine lining, leading to spotting between periods in perimenopause. Brown discharge can also be a sign of vaginal atrophy, in which thinning vaginal walls lead to minor bleeding. However, persistent or foul-smelling discharge should be evaluated for infections or other gynecological concerns.
8. How can I manage frequent perimenopausal bleeding?
Managing frequent perimenopausal bleeding often involves lifestyle modifications, hormone therapy, or medical interventions. Maintaining a balanced diet rich in iron and vitamin C can help counteract anemia caused by heavy bleeding. Stress management techniques, such as yoga and meditation, can help regulate hormones. For those experiencing a perimenopause period every two weeks or spotting all month, low-dose birth control pills or progesterone therapy may help regulate cycles. In severe cases, procedures such as endometrial ablation or a hormonal IUD can help reduce excessive bleeding.
9. What does it mean if I have perimenopausal bleeding between periods?
Perimenopausal bleeding between periods is usually linked to hormonal fluctuations, but it can also be a sign of fibroids, endometrial polyps, or infections. Some women experience perimenopause spotting instead of a period due to erratic ovulation patterns. Spotting between periods in perimenopause may also result from changes in the cervix, such as cervical polyps, which are typically benign but may need removal. If spotting becomes frequent, heavy, or is accompanied by pain, a pelvic exam or ultrasound may be necessary to rule out serious conditions.
10. Can I still get pregnant if I am experiencing perimenopause spotting?
Yes, pregnancy is still possible during perimenopause, even if your periods are irregular or you are experiencing perimenopause spotting instead of a period. Ovulation may become unpredictable, but as long as the ovaries continue to release eggs, conception can occur. Women who do not wish to become pregnant should continue using contraception until they have gone a full year without a menstrual cycle. If you are experiencing perimenopause spotting all month and suspect pregnancy, taking a test can clarify the situation. Consulting a healthcare provider can help assess fertility status and discuss family planning options.
Conclusion: Navigating Perimenopausal Bleeding with Confidence
Perimenopausal bleeding can be unpredictable and sometimes alarming, but understanding the changes occurring in the body can empower women to navigate this phase with confidence. Recognizing what is normal—such as spotting between periods, occasional heavy bleeding, or periods getting closer together in their 40s—versus when to seek medical advice is essential for maintaining health and well-being.
By staying informed about the causes and management options for perimenopausal bleeding, women can make educated decisions about their health. Whether opting for lifestyle changes, medical treatments, or a combination of both, understanding the body’s signals and taking proactive steps can ensure a smoother transition into menopause. If symptoms such as prolonged bleeding, frequent spotting, or intense pelvic pain arise, consulting a healthcare provider is the best course of action. Ultimately, being proactive about perimenopausal health fosters confidence, peace of mind, and overall well-being during this natural stage of life.
Further Reading:
Perimenopausal Bleeding – What’s Normal?
perimenopause symptoms, irregular periods in 40s, hormonal changes in menopause, menopause transition, heavy menstrual bleeding causes, abnormal uterine bleeding, endometrial health, estrogen fluctuations, progesterone imbalance, midlife menstrual cycle, spotting after period, menstrual health in aging, female reproductive health, prolonged periods causes, hormonal therapy for menopause, natural remedies for perimenopause, gynecological health, menopause and bleeding, women’s hormonal balance, uterine lining changes
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While News7Health strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. News7Health, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of News7Health.

